|
The interpretation of the
fetal heart rate tracing should follow a systematic approach with a full
qualitative and quantitative description of the following:
-
Baseline rate
-
Baseline fetal heart rate (FHR) variability
-
Presence of accelerations
-
Periodic or episodic decelerations
-
Changes or trends of FHR patterns
over time
-
Frequency and intensity of uterine contraction
Baseline Fetal Heart Rate (FHR):
The baseline FHR is the heart rate during a 10 minute segment rounded to the nearest 5
beat per minute
increment excluding periods of marked FHR variability, periodic or episodic
changes, and segments of baseline that differ by more than 25 beats per
minute.
The minimum baseline duration must be at least 2 minutes.
If minimum baseline duration is < 2 minutes
then the baseline is indeterminate.
Bradycardia
:Mean FHR < 110 BPM
-
A rate of 100-119 BPM in the absence
of other non reassuring patterns is not usually a sign of compromise[ 4]
-
Etiologies: Heart block (little
or no variability), occiput posterior or transverse position, serious
fetal compromise.
Tachycardia:
Mean FHR>160 BPM
-
In the presence of good variability
tachycardia is not a sign of fetal distress [4]
-
Etiologies: Maternal fever, fetal
hypoxia, fetal anemia, amnionitis, fetal tachyarrhythmia (usually > 200
BPM with abrupt onset little to no variability) SVT (200-240 BPM) [5] ,
fetal heart failure, drugs (beta sympathomimetics, vistaril, phenothiazines)
, rebound ( transient tachycardia following a deceleration accompanied
by decreased variability) [4]
Baseline change:
The decrease or increase in heart rate lasts for longer than 10 minutes.
Baseline FHR Variability
Baseline variability is defined as fluctuations in the fetal heart rate of
more than 2 cycles per minute. No distinction is made between short-term
variability (or beat-to-beat variability or R-R wave period differences
in the electrocardiogram) and long-term variability.
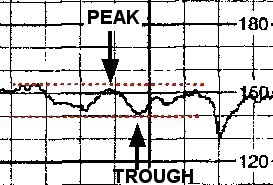
Grades of fluctuation are based
on amplitude range (peak to trough):
|
Absent variability = Amplitude
range undetectable
Minimal = < 5 BPM
Moderate = 6 to 25 BPM
Marked = > 25 BPM
The tracing to the right shows an amplitude range of ~ 10 BPM (moderate
variability ).
|
 |
A sinusoidal pattern has regular
amplitude and frequency and is excluded in the definition of variability.A sinusoidal pattern "Visually apparent, smooth, sine wave-like undulating pattern in FHR baseline with a cycle frequency of 3-5 per minute which persists for 20 minutes or more.”.. Variability is absent. This pattern has been associated with severe fetal anemia. [6]
Persistently minimal or absent FHR variability appears to be the most
significant intrapartum sign of fetal compromise [32]. On the other hand the
presence of good
FHR variability may not always be predictive of a good outcome.[33].
-
Etiologies of decreased variability:
Fetal metabolic acidosis [7], CNS depressants[8,9], fetal sleep cycles[10],
congenital anomalies, prematurity [11,12], fetal tachycardia, preexisting
neurologic abnormality [13], normal [14], betamethasone[15].
Accelerations
An acceleration is an abrupt increase in FHR above baseline with onset to peak of
the acceleration less than < 30 seconds and less than 2 minutes in duration. The duration of the acceleration is defined
as the time from the initial change in heart rate from the baseline to the time
of return to the FHR to baseline.
Adequate accelerations are
defined as:
-
<32 weeks' : >10 BPMabove baseline for
>10 seconds [3]
-
>32 weeks' : >15 BPM above
baseline for > 15 seconds[3].
Prolonged acceleration:
Increase in heart rate lasts for 2 to 10 minutes.
The absence of accelerations for more than 80 minutes correlates with increased
neonatal morbidity [38,39].
Fetal scalp stimulation can be used to induce accelerations.
There is about a 50% chance of acidosis in the fetus who fails to respond
to stimulation in the presence of a nonreassuring pattern [17].
This technique should not be used to verify the absence of acidemia during a deceleration of the FHR
since there is insufficient literature to support its use during a
deceleration.
|
REACTIVITY[16]*
An increase of 15 BPM
above baseline for 15 second duration (from baseline to baseline) twice in a 20 minute period.
Since the amplitude
of accelerations is inversely proportional to the rate premature fetuses
often do not meet criteria for reactivity.
Only 65% of fetuses
at 28 weeks are reactive by this criteria.
By 34 weeks 95% of fetuses
are reactive.
*Reactivity ( a term used in
antenatal testing) is not defined
by the NIHCD guidelines.
|
Periodic or episodic decelerations
Episodic patterns are those
not associated with uterine contractions .
Periodic patterns are those
associated with uterine contractions.
-
Early and late decelerations (with
some exceptions-i.e., supine hypotension) are periodic.
-
Variables can also be periodic.
Quantitated by the depth
of the nadir in BPM below the baseline.The duration is quantitated in minutes
and seconds from the beginning to the end of the deceleration. (Accelerations
are quantitated similarly.)
The type of the deceleration
is distinguished on the basis of its waveform.
Gradual decrease and return
to baseline with time from onset of the deceleration to nadir >30
seconds.
-
Further subclassified based on
their relation to the contraction.
Abrupt decrease in FHR of > 15 beats per
minute
with onset of deceleration to nadir < 30 seconds.
|
Early deceleration:
Gradual decrease in FHR
with onset of deceleration to
nadir >30 seconds. The nadir occurs with the peak
of a contraction. |
 |
|
Late Deceleration:
Gradual decrease in FHR
with onset of deceleration
to nadir >30 seconds. Onset of the decleration occurs after the
beginning of the contraction, and the nadir of the contraction occurs after
the peak of the contraction. |
 |
|
Variable:
Abrupt decrease in FHR of > 15 beats per
minute measured from the most recently determined baseline rate.
The onset of deceleration
to nadir is less than 30 seconds. The deceleration lasts > 15 seconds and less than 2 minutes.
A shoulder, if present, is not included as part of
the deceleration.
|
 |
Recurrent decelerations ( variable, early,
or late ): Decelerations occur with > 50% of uterine contractions in
any 20 minute segment.
Prolonged deceleration : A
decrease in FHR of > 15 beats per
minute measured from the most recently determined baseline rate.
The deceleration lasts
>= 2 minutes but less than 10 minutes.
-
Etiologies: Maternal hypotension
[18] , uterine hyperactivity, cord prolapse, cord compression, abruption,
artifact (maternal heart rate) , maternal seizure [19]
Although umbilical cord compression is often responsible
for a prolonged deceleration a pelvic examination should be performed
to rule out umbilical cord prolapse or rapid descent of the fetal head.[4]
Late
Decelerations
Late decelerations associated with preservation
of beat-to beat variability
These decelerations appear to
be mediated by arterial chemo receptors in mild hypoxia.
When the level of oxygen in the fetal blood
is below a pO2 of 15-20 mm Hg chemoreceptors
are triggered causing reflex alpha adrenergic stimulation which constricts
blood vessels in nonvital peripheral
areas such as the arms and legs to divert more blood flow to vital organs such
as the heart and brain. Constriction of
peripheral blood vessels leads to hypertension.
The
hypertension stimulates a baroreceptor mediated vagal response that slows the
heart rate. [20] .
Late decelerations associated with no variability
(where loss of variability has not been caused by drug administration)
If the supply of oxygen continues to be limited (hypoxia) , the peripheral
tissues cannot completely break down glucose and instead convert it to lactic
acid.
Significant levels of acid in the blood (acidemia) may suppress the fetal
nervous system which becomes evident as decreased variability.
As acidosis develops the brain
stem reflexes become blunted and direct myocardial depression causes shallow
decelerations [20,22].
If myocardial depression is severe
enough, lates may be absent all together [22].
Management of Late Decelerations
These maneuvers are primarily
intended to alleviate "reflex" lates.
Place patient on side [23,24]
Discontinue oxytocin.
Correct any hypotension
IV hydration.
If decelerations are associated with tachysystole
consider terbutaline 0.25 mg SC [26,27]
Administer O2 by tight face mask
[25, 40]
If late decelerations persist
for more than 30 minutes despite the above maneuvers, fetal scalp pH is
indicated.
Scalp pH > 7.25 is reassuring,
pH 7.2-7.25 may be repeated in 30 minutes.
Deliver for pH < 7.2
or minimal baseline variability with late or prolonged decelerations
and inability to obtain fetal scalp pH [28,29]
The observation of
recurrent late decelerations with minimal or absent variability should lead to consideration of
expeditious delivery unless the
abnormal results are believed to be the result of a reversible maternal
condition such as diabetic ketoacidosis or pneumonia with hypoxemia.
Variable
Decelerations

Vagally mediated through chemoreceptors
or baroreceptors.
Accelerations "shoulders" before
and after a variable deceleration are thought to be caused by partial cord
occlusion .Decreased venous return causes a baroreceptor-mediated acceleration.
Hypertension and decreased arterial
oxygen tension secondary to complete cord occlusion results in deceleration.
Variables occur with head compression
secondary to vagal nerve activation, and with movement in the premature
fetus[30]
The timing of the deceleration
may occur periodically either with or after the contraction [31].
Management of Variables
Change position to where FHR pattern
is most improved. Trendelenburg may be helpful.
Discontinue oxytocin.
Check for cord prolapse or imminent
delivery by vaginal exam.
Consider amnioinfusion[35-37]
Administer 100% O2 by tight face mask [4].
Uterine Contractions [41]
Uterine contractions are quantified as the number of contractions present in a 10-minute window, averaged over 30 minutes.
Normal: 5 or less contractions in 10 minutes, averaged over a
30-minute window.
Tachysystole: More than 5 contractions in 10 minutes, averaged
over a 30-minute window. Applies to both spontaneous or stimulated labor. Tachysystole should always be qualified as to the presence or
absence of associated FHR decelerations.
The terms hyperstimulation and hypercontractility are not defined and should no longer be used.
Three-Tier Fetal Heart Rate Interpretation System [41]
Category I : Normal.
The fetal heart rate tracing shows ALL of the following:
Baseline FHR 110-160 BPM, moderate FHR variability, accelerations may be present or
absent, no late or variable decelerations, may have early decelerations.
Strongly predictive of normal acid-base status at the time of observation.
Routine care.
Category II : Indeterminate.
The fetal heart rate tracing shows ANY of the following:
Tachycardia, bradycardia without absent variability, minimal variability, absent
variability without recurrent decelerations, marked variability, absence
of accelerations after stimulation, recurrent variable decelerations with
minimal or moderate variability, prolonged deceleration > 2minute but
less than 10 minutes, recurrent late decelerations with moderate variability,
variable decelerations with other characteristics such as slow return to
baseline, and "overshoot".
Not predictive of abnormal fetal acid-base status, but
requires continued surveillance and reevaluation.
Category III: Abnormal.
The fetal heart rate tracing shows EITHER of the following:
Sinusoidal pattern OR absent variability with recurrent late
decelerations,
recurrent variable decelerations, or bradycardia.
Predictive of abnormal fetal-acid base status at the time of observation.
Depending on the clinical situation, efforts to expeditiously resolve the underlying cause of the abnormal fetal heart rate pattern should be made.
SEE ALSO
- The use of electronic fetal monitoring: the use and interpretation of cardiotocography in
intrapartum fetal surveillance. Evidence-based clinical guideline number 8. Clinical Effectiveness
Support Unit. London (UK): RCOG Press; 2001. Available at:
www.rcog.org.uk/resources/public/pdf/efm_guideline_final_2may2001.pdf.
- Liston R, Sawchuck D, Young D. Society of Obstetrics and
Gynaecologists of Canada, British Columbia Perinatal Health Program.
Fetal health surveillance: antepartum and intrapartum consensus guideline [published
erratum appears in J Obstet Gynaecol Can 2007;29:909]. J Obstet Gynaecol Can
2007;29 suppl:S3–56.
REFERENCES
1. Renou P, Warwick N, Wood C :Autonomic control of fetal heart rate. Am J Obstet Gynecol 105:949,1969
PUBMED
2. Gagnon R, Campbell K, Hunse C, Patrick J Patterns of human fetal heart rate accelerations from 26 weeks
to term. Am J Obstet Gynecol. 1987 Sep;157(3):743-8.
PUBMED
3.Electronic
fetal heart rate monitoring: research guidelines for interpretation. National
Institute of Child Health and Human Development Research Planning Workshop.
Am J Obstet Gynecol. 1997 Dec;177(6):1385-90.
PUBMED
4.American
College of Obstetricians and Gynecologists. Fetal Heart Rate Patterns:
Monitoring, Interpretation, and Management. ACOG
Technical Bulletin 207. Washington, DC: ACOG, 1995
5. Hobel CJ Intrapartum clinical assessment of fetal distress. Am J Obstet Gynecol. 1971 Jun 1;110(3):336-42.
PUBMED
6. ACOG Practice Bulletin No. 106: Intrapartum fetal heart rate monitoring: nomenclature, interpretation, and general management principles. Obstet Gynecol. 2009 Jul;114(1):192-202 7. Paul RH, Suidan AK,
Yeh S, Schifrin BS, Hon EH Clinical fetal monitoring. VII. The evaluation
and significance of intrapartum baseline FHR variability. Am J Obstet Gynecol.
1975 Sep 15;123(2):206-10.
PUBMED
8.Petrie RH, Yeh SY,
Murata Y, Paul RH, Hon EH, Barron BA, Johnson RJ The effect of drugs on
fetal heart rate variability. Am J Obstet Gynecol. 1978 Feb 1;130(3):294-9.
PUBMED
9. Babaknia A, Niebyl JRThe effect of magnesium sulfate
on fetal heart rate baseline variability. Obstet Gynecol. 1978 Jan;51(1
Suppl):2s-4s.
PUBMED
10. Visser GH, Goodman JD, Levine DH, Dawes GSDiurnal
and other cyclic variations in human fetal heart rate near term. Am J Obstet
Gynecol. 1982 Mar 1;142(5):535-44.
PUBMED
11. Devoe LD Antepartum fetal heart rate testing in
preterm pregnancy. Obstet Gynecol. 1982 Oct;60(4):431-6.
PUBMED
12.Assali NS, Brinkman
CR 3d, Woods JR Jr, Dandavino A, Nuwayhid B Development of neurohumoral
control of fetal, neonatal, and adult cardiovascular functions. Am J Obstet
Gynecol. 1977 Dec 1;129(7):748-59.
PUBMED
13. van der Moer PE,
Gerretsen G, Visser GH Fixed fetal heart rate pattern after intrauterine
accidental decerebration. Obstet Gynecol. 1985 Jan;65(1):125-7.
PUBMED
14. Smith JH, Dawes GS, Redman
CW Low human fetal heart rate variation in normal pregnancy. Br J Obstet
Gynaecol. 1987 Jul;94(7):656-64.
PUBMED
15. Derks JB, Mulder EJ, Visser GH The effects of
maternal betamethasone administration on the fetus. Br J Obstet Gynaecol.
1995 Jan;102(1):40-6.
PUBMED
16. Evertson LR, Gauthier RJ,
Schifrin BS, Paul RH Antepartum fetal heart rate testing. I. Evolution
of the nonstress test.Am J Obstet Gynecol. 1979 Jan 1;133(1):29-33.
PUBMED
17. Smith CV, Nguyen HN, Phelan JP, Paul RH. Intrapartum
assessment of fetal well-being: a comparison of fetal acoustic stimulation
with acid-base determinations. Am J Obstet Gynecol 1986;155:726-728
PUBMED
18. Hon EH, Reid BL, Hehre FW: The electronic evaluation
of the fetal heart rate II. Changes with maternal hypotension. Am J Obstet
Gynecol 79:209, 1960
19.Boehm FH, Growdon
JH Jr The effect of eclamptic convulsions on the fetal heart rate. Am J
Obstet Gynecol. 1974 Nov 15;120(6):851-2.
PUBMED
20. Harris JL,
Krueger TR, Parer JT Mechanisms of late decelerations of the fetal heart
rate during hypoxia. Am J Obstet Gynecol. 1982 Nov 1;144(5):491-6.
PUBMED
21. Murata Y, Martin
CB Jr, Ikenoue T, Hashimoto T, Taira S, Sagawa T, Sakata H Fetal heart
rate accelerations and late decelerations during the course of intrauterine
death in chronically catheterized rhesus monkeys. Am J Obstet Gynecol.
1982 Sep 15;144(2):218-23.
PUBMED
22. Gaziano EP,
Freeman DW Analysis of heart rate patterns preceding fetal death. Obstet
Gynecol. 1977 Nov;50(5):578-82. PMID:
PUBMED
23. Abitbol MM. Supine position
in labor and associated fetal heart rate changes. Obstet Gynecol 1985;65:481-486
24. Clark SL, Cotton DB, Pivarnik
JM, Lee W, Hankins GDV, Benedetti TJ, et al. Position change andcentral
hemodynamic profile during normal third-trimester pregnancy and post partum.
Am J Obstet Gynecol 1991;164: 883-887
25. Willcourt RJ, King JC,
Queenan JT: Maternal oxygenation administration and the fetal transcutaneous
PO2. Am J Obstet Gynecol. 1983 Jul 15;146(6):714-5.
PUBMED
26. Arias F. Intrauterine resuscitation
with terbutaline: a method for the management of acute intrapartum
fetal distress. Am J Obstet Gynecol 1978;131:39-43
27. Reece EA, Chervenak FA, Romero R, Hobbins JC. Magnesium sulfate in the management of acute
intrapartum fetal distress. Am J Obstet Gynecol 1984;148:104-107
28. In Freeman RK, Garite TJ, Nageotte MP, Fetal Heart Rate Monitoring,
3rd ed. ,Williams & Wilkins , 2003
29. Low JA, Victory R, Derrick EJPredictive value
of electronic fetal monitoring for intrapartum fetal asphyxia with metabolic
acidosis. Obstet Gynecol. 1999 Feb;93(2):285-91.
PUBMED
30. Timor-Tritsch IE, Dierker LJ, Zador I, Hertz
RH, Rosen MGFetal movements associated with fetal heart rate accelerations
and decelerations. Am J Obstet Gynecol. 1978 Jun 1;131(3):276-80.
;
PUBMED
31. Young BK, Katz M, Wilson SJ Fetal blood and tissue pH with variable deceleration patterns. Obstet
Gynecol. 1980 Aug;56(2):170-5.
PUBMED
32.Williams KP and Galerneau F. Intrapartum fetal heart rate patterns in the prediction of neonatal acidemia. Am J Obstet Gynecol.200;188(3):820-3.
PUBMED
33. Samueloff A, Langer O, Berkus M, Field N,
Xenakis E, Ridgway L.Is fetal heart rate variability a good predictor of fetal outcome?
Acta Obstet Gynecol Scand.1994;73(1):39-44.
PUBMED
35. Miyazaki FS, Nevarez F.
Saline amnioinfusion for relief of repetitive variable decelerations: a
prospective randomized study. Am J Obstet Gynecol 1985;153:301-306
36. Nageotte MP, Freeman RK, Garite TJ, Dorchester W. Prophylactic intrapartum amnioinfusion inpatients
with preterm premature rupture of membranes. Am J Obstet Gynecol 1985;153:557-562
37. Strong TH Jr, Hetzler G,
Sarno AP, Paul RH. Prophylactic intrapartum amnioinfusion: a randomized
clinical trial. Am J Obstet Gynecol
38.Patrick J ,et al. , Accelerations of the human fetal heart rate at 38
to 40 weeks' gestational age.Am J Obstet Gynecol.1984 Jan 1;148(1):35-41
PUBMED
39.Luerti M, et al Accelerations in greater than intra-partum greater
than cardiotocographic recording I. Correlation with perinatal outcome.
Clin Exp Obstet Gynecol.1980;7(2):94-100.
PUBMED
40.Haydon ML, et al. The effect of maternal oxygen administration on fetal pulse
oximetry during labor in fetuses with nonreassuring fetal heart rate patterns.
Am J Obstet Gynecol September 2006;195:735-8.PUBMED
41. Macones GA et al., The 2008 National Institute of Child Health and Human
Development Workshop Report on Electronic Fetal MonitoringUpdate on Definitions, Interpretation, and Research Guidelines Obstetrics &
Gynecology 2008;112:661-666 PMID:18757666
|

